Role of Patient Reported Outcomes in the era of Precision Medicine
The rapid technological evolution of smartphone and sensory devices over the last few years are significantly improving the sophistication of mobile apps, and are expanding the range and potential of ePROs (Electronic patient reported outcomes). Some mobile apps and sensors can be adapted and used as ePRO tools to collect Vital Signs (VS) data, Quality of Life Questionnaires, or disease specific patient diaries, all of which can be completed by the patient.
The National Quality Forum (NQF) defines PROs as “any report of the status of a patient’s health condition that comes directly from the patient, without interpretation of the patient’s response by a clinician or anyone else.” PRO tools enable the assessment of patient–reported health data for physical, mental, and social well–being. Patients feel like an integral part of the care team when they can contribute to the decision-making process.
ePRO data is different from those collected in a clinical setting in two ways:
- Patients, are primarily responsible for capturing or recording these data.
- Patients have the freedom to decide how to share or distribute these data to healthcare providers and others.
Advantages of ePROs
- Supplement existing clinical data, filling in gaps in information and providing a more comprehensive picture of ongoing patient health.
- Provide important information about how patients are doing between medical visits.
- Gather information on an ongoing basis—rather than just one point in time—and provide information relevant to preventive and chronic care management.
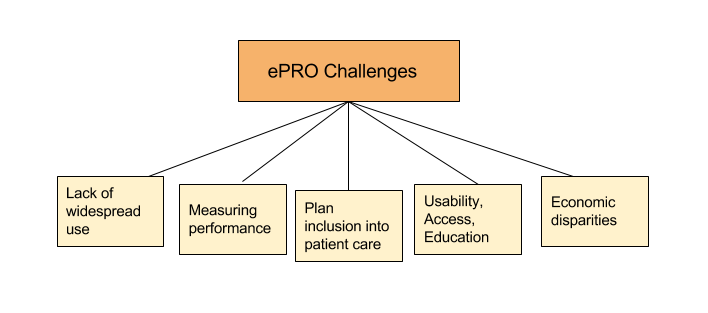
ePRO Challenges
- They are not in widespread use in clinical practice.
- Little is known about aggregating this data for measuring performance of the health system delivering care.
- Providers must determine when and how these data are included in the medical record and care plan.
- Usability, access, education, and other social issues must be addressed to achieve widespread patient use.
- Economic disparities must be overcome.
Patient-generated health data does more than just add more information to an EHR – it changes the way providers interact with their patients outside of the hospital, helps healthcare experts develop new treatment plans, and even makes the patient feel like an important partner in care.
By supporting patient-generated health data collection, providers are able to better the healthcare industry by helping build a wealth of information clinicians, researchers, and patients can all use.
Boost to the Precision Medicine Initiative
Patient-generated health data also plays a critical role in the Precision Medicine Initiative (PMI). It calls for patients to volunteer their health data to clinical analysts and researchers to develop optimized treatment plans. In fact, patient-generated health data is arguably the crux of PMI. Alongside an array of EHR data, PMI operates off of patient-generated health data and health data contributed by patients themselves.
However, in order to make this happen, it’s important that patient data sharing and patient access to data is widely available.
With the increased consumer adoption of technology, patients can take ownership and better manage their healthcare including electronic data capture modes of PROs (Patient Reported Outcomes) via Apple’s ResearchKit and Applied Informatic’s ResearchDroid powered study apps. This offers a host of exciting opportunities to learn from patients’ experiences throughout their journey. Let us look at some examples of studies using mobile research apps for precision medicine.
Citizen Endo’s Endometriosis Study App – Phendo
Citizen Endo is conducting an observational study of patient reported outcomes relevant to the patients’ experience through time, as collected through a novel smartphone app – Phendo (Developed by Applied Informatics). Endometriosis remains a mysterious disease. In particular, there exists a gap between physicians’ mental model of the disease and the patient experience of endometriosis. The app is now collecting patient-reported data from endometriosis patients, creating the first dataset of patient experience of endometriosis tracked by patients themselves through time. Collection of this type of data provides a comprehensive and rich dataset for the research community. Identifying potential clusters of patients from their signs and symptoms, and comorbidities furthers what is known about disease subtypes and is a good first step towards precision medicine for endometriosis.
Novartis’ Multiple Sclerosis App – ElevateMS
Novartis Pharmaceuticals has launched a mobile research study for people with multiple sclerosis that collects data via their smartphones. This does away with clinic visits typically associated with such research studies.
The study, “Evaluation of Evidence from Smart Phone Sensors and Patient-Reported Outcomes in Participants with Multiple Sclerosis,” or ElevateMS, is designed to collect smartphone sensor-based data from physical tasks and symptoms.
The goal of the study is to improve understanding of the daily challenges patients with MS can have and to uncover new potential measurements of treatment effectiveness through real-time data collection from participants in their everyday life. Using smartphones, the elevateMS app will capture participant responses to questionnaires, passive and active sensor-based movement data, and functional performance tasks completed by the participants.n turn, this data may provide researchers with new ways to look at disease progression and treatment effectiveness.
Stanford University’s MyHeart Counts 2.0 App
One of the first apps to be introduced on Apple’s ResearchKit platform two years ago, the Stanford University School of Medicine’s MyHeart Counts app has logged more than 54,000 participants in a research project that focuses on heart health. Now comes MyHeart Counts 2.0, which combines mHealth with precision medicine to give the user a personalized care management plan.
mHealth advocates see this as the next phase in app development, which moves to combine biometric monitoring with analytics tools and artificial intelligence to move from collecting to coaching. Through MyHeart Counts 2.0, users share their data on day-to-day activity levels, cardiovascular health, blood pressure and cholesterol levels. Stanford takes that data and pushes it back to the user in the form of a personal health plan called the Stanford Coaching Module. The plan includes a week of baseline measurements, then four one-week-long behavior change interventions that are based on comparing the user’s health data to population health metrics.
Data is the fuel of precision medicine, making all the parts of the complex engine work together to find the right course of treatment. The White House-sponsored Precision Medicine Initiative too calls for the combination of massive amounts of patient generated health data, information generated by clinicians, and genomic data to better assess the efficacy of treatments and to optimize plans of care for patients.